Camosten™ (14 pcs.)
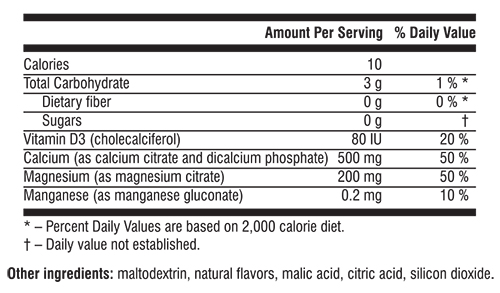
Camosten™ is easily blended with water or juice and quickly absorbed by the body due to the combination of bioactive forms of calcium and magnesium (citrates), vitamin D (cholecalciferol) and manganese. The product is highly bioavailable.
The product has been manufactured using high quality pure raw materials and the technology that ensures all their beneficial properties intact, in strict compliance with GMP and TÜV regulations.
Camosten™ is a unique Santegra®’s product, which is easily blended with liquid and quickly absorbed by the body. Calcium is combined with magnesium, manganese and vitamin D to give you the ultimate support for healthy bones, improves teeth and hair condition.
“You are not what you eat; you are what you absorb”. What’s the point in eating handfuls of calcium tablets if your body cannot absorb it? Calcium assimilability is the most important index while comparing different calcium forms.
Camosten™ contains calcium citrate, which is one of the most bioavailable forms of calcium. Calcium citrate consumption doesn’t impair blood biochemical parameters and doesn’t increase the risk of kidney stone formation. Camosten™ contains 500 mg calcium per packet.
Calcium is vital for the formation of strong bones and teeth and for the healthy gums, prevents bone loss associated with osteoporosis. It is also important in the maintenance of healthy cardiovascular system and the transmission of nerve impulses, for muscular growth and contraction, and for the prevention of muscle cramps.
The results of several clinical trials showed that the regular and long-term consumption of adequate calcium prevents bone loss and fraction. (1,2)
Calcium supplementation helps to reduce the risk of heart diseases in menopausal women. (3)
Calcium also appears to partially bind some fats and cholesterol in the gastrointestinal tract. Perhaps as a result, some research suggests that calcium supplementation may help lower cholesterol levels. (4)
The main source of calciumis food and if the intake is not adequate, calcium is absorbed from the bones.
Most people eat well below the recommended amount of calcium. This lack of dietary calcium is thought to contribute to the risk of osteoporosis, which nowadays is considered to be a “hidden epidemic”. About 30% of population (mostly women) has osteoporosis at the age of 50 and almost 50% - at the age of 70.
Vitamin D works with calcium to build strong bones and teeth.
The fat-soluble vitamin D’s most important role is maintaining levels of calcium and phosphorus. The majority of vitamin D in the body is created during a chemical reaction that starts with sunlight exposure to the skin. Vitamin D is often called “sun vitamin”.
The main biological function of vitamin D is maintaining the calcium and phosphorus balance. Vitamin D plays a vital role in calcium and phosphorus absorption, which is essential for the strong bones. Vitamin D helps to fight rickets, supports the immune system.
Magnesium is an essential mineral for human health with a wide range of biological functions. Magnesium activates more than 300 enzymes in the body. Magnesium plays important role in bone health, increasing calcium absorption, has anti-osteoporotic activity. Magnesium is considered the "antistress" mineral: it relaxes nerves and muscles. Magnesium, in combination with calcium, helps regulate nerve and muscle tone.
Manganese is an essential trace mineral needed for healthy skin, bones and cartilage formation and maintenance. Manganese is involved in metabolism of carbohydrates, fats and proteins, has antioxidant activity, protects the body against damage from free radicals.
The benefit of Camosten™ is that it does not contain sugar, which makes it available for diabetics, and everyone who is concerned about excess sugar consumption.
Add contents of 1 packet to 200 ml of water or juice and drink immediately. Use once or twice daily.
Contraindication
Individual intolerance.
Calcium
Calcium, the most abundant mineral in the human body, has several important functions. More than 99% of total body calcium is stored in the bones and teeth where it functions to support their structure. (5)
The remaining 1% is found throughout the body in blood, muscle, and the fluid between cells. Calcium is needed for muscle contraction, blood vessel contraction and expansion, the secretion of hormones and enzymes, and sending messages through the nervous system.
A constant level of calcium is maintained in body fluid and tissues so that these vital body processes function efficiently.
It is important to get plenty of calcium in the foods you eat. Foods rich in calcium include diary products such as milk, cheese and yogurt, and leafy, green vegetables. The exact amount of calcium you need depends on your age and other factors. Growing children and teenagers need more calcium than young adults. Older women need plenty of calcium to prevent osteoporosis. People who do not eat enough high-calcium foods should take a calcium supplement.
Bone undergoes continuous remodeling, with constant resorption (breakdown of bone) and deposition of calcium into newly deposited bone (bone formation). The balance between bone resorption and deposition changes as people age. During childhood there is a higher amount of bone formation and less breakdown. In early and middle adulthood, these processes are relatively equal. In aging adults, particularly among postmenopausal women, bone breakdown exceeds its formation, resulting in bone loss, which increases the risk for osteoporosis (a disorder characterized by porous, weak bones).
Bones continue to add more mass until around age 30, when peak bone mass is reached. Because bone loss, like bone growth, is a gradual process, the stronger your bones are at age 30, the more your bone loss will be delayed as you age. Therefore, it is particularly important to consume adequate calcium and vitamin D throughout infancy, childhood, and adolescence. It is also important to engage in weight-bearing exercise to maximize bone strength and bone density (amount of bone tissue in a certain volume of bone) to help prevent osteoporosis later in life.
Weight bearing exercise is the type of exercise that causes your bones and muscles to work against.
Examples of weight bearing exercise: walking, running, dancing, aerobics, skating.
Osteoporosis is a disorder characterized by porous, fragile bones. Osteoporosis is a serious public health problem for more than 10 million Americans, 80% of whom are women. Another 34 million Americans have osteopenia, or low bone mass, which precedes osteoporosis. Osteoporosis is a concern because of its association with fractures of the hip, vertebrae, wrist, pelvis, ribs, and other bones. Each year, Americans suffer from 1.5 million fractures because of osteoporosis. (6)
When calcium intake is low or calcium is poorly absorbed, bone breakdown occurs because the body must use the calcium stored in bones to maintain normal biological functions such as nerve and muscle function. Bone loss also occurs as a part of the aging process. A prime example is the loss of bone mass observed in post-menopausal women because of decreased amounts of the hormone estrogen. Researchers have identified many factors that increase the risk for developing osteoporosis. These factors include being female, thin, inactive, of advanced age, cigarette smoking, excessive intake of alcohol, and having a family history of osteoporosis. (7)
Researches show that calcium supplementation is essential for the osteoporosis prevention. (29, 30, 31)
Some observational and experimental studies indicate that individuals who eat a vegetarian diet high in minerals (including calcium, magnesium and potassium) and fiber, and low in fat, tend to have reduced blood pressure. (8, 9, 10)
Findings from some clinical trials (a specific type of experimental study) used to evaluate the effects of one or more treatments/interventions in humans) indicate that an increased calcium intake lowers blood pressure and the risk of hypertension (high blood pressure). (11, 12)
Several studies, primarily observational in nature, have linked higher calcium intakes to lower body weights or less weight gain over time. (13, 14, 15)
Magnesium
There are about 19 g of Mg in the average 70 kg adult body, of which approximately 65% is found in bone and teeth, and the rest is distributed between the blood, body fluids, organs and other tissue. Magnesium is involved in the synthesis of protein, and it is an important co-factor in more than 300 enzymatic reactions in the human body, many of which contribute to the production of energy, and with cardiovascular functions. While calcium affects muscle contractions, magnesium balances that effect and relaxes muscles. Most of magnesium is inside the cell, and while iron is the central atom in hemoglobin, magnesium is the central core of the chlorophyll molecule in plant tissue
Vitamin D
Vitamin D (calciferol) is photosynthesized in the skin by the action of solar ultraviolet B radiation. Vitamin D comes in many forms, but the two major physiologically relevant ones are vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol) (Fieser and Fieser, 1959).
Vitamin D’s major biologic function in humans is to maintain serum calcium and phosphorus concentrations within the normal range by enhancing the efficiency of the small intestine to absorb these minerals from the diet
Vitamin D is essential for the efficient utilization of calcium by the body. (17)
There is plenty of scientific evidence that vitamin D has several different effects on immune system function. (18)
The active form of vitamin D plays a role in insulin secretion under conditions of increased insulin demand. Limited data in humans suggests that insufficient vitamin D levels may have an adverse effect on insulin secretion and glucose tolerance in type 2 diabetes. (19, 20)
Adequate vitamin D levels may be important for decreasing the risk of high blood pressure.
Osteoporosis is most often associated with inadequate calcium intake. However, a deficiency of vitamin D also contributes to osteoporosis by reducing calcium absorption. While rickets and osteomalacia are extreme examples of vitamin D deficiency, osteopororsis is an example of a long-term effect of vitamin D insufficiency. Adequate storage levels of vitamin D help keep bones strong and may help prevent osteoporosis in older adults, in those who have difficulty walking and exercising, in post-menopausal women, and in individuals on chronic steroid therapy. (21, 22, 23)
Several studies suggest that a higher dietary intake of calcium and vitamin D correlates with lower incidence of cancer. (24, 25)
Since a large body of science shows vitamin D works closely with calcium and magnesium, it is best to take your vitamin D in combination with calcium and magnesium to maintain a proper balance. Recent literature also shows most calcium supplements have too little vitamin D to be effective. And some of them use synthetic vitamin D2. A much better form is natural vitamin D3 which stays in your system longer and with more effect.
Camosten™ is a well balanced combination of the natural form of vitamin D – cholecalciferol, calcium and magnesium for the ultimate protection if your bones.
A randomized, placebo-controlled study documented that calcium citrate supplementation averts bone loss and stabilizes bone density in early postmenopausal women.
Doctor Khashayar Sakhaee and co-authors at the Center for Mineral Metabolism and Clinical Research, University of Texas Southwestern Medical Center, Dallas, Texas conducted a clinical study to evaluate the effect of calcium supplements on the early stages of osteoporosis.
In the two-year study, 63 healthy, postmenopausal women were separated into two groups - 29 subjects were allocated to the calcium citrate group (were given 400 mg of calcium citrate twice a day) and 34 - to the placebo group. Those in the placebo group took tablets of identical appearance. Bone density was tested at three sites most commonly affected by osteoporosis: the vertebrae in the lower back (spine), the radial shaft (wrist) and the femoral neck (hip). The data indicates:
Calcium citrate supplementation preserved bone mass in the spine, femoral neck, and radial shaft in a group comprised mostly of early postmenopausal women during two years of the trial. The difference in the bone mass between the two groups was significant after two years of calcium citrate treatment.
In another study was evaluated the effect of calcium citrate supplementation on the stone forming propensity in healthy postmenopausal women.
A total of 18 postmenopausal women without stones underwent a randomized trial. During the last 2 days of each phase urine was collected in 24-hour pools for complete stone risk analysis.
Conclusions: Calcium citrate supplementation does not increase the risk of stone formation in healthy postmenopausal women. (26)
An analysis of 15 randomized trials concluded that calcium citrate was absorbed 22% to 27% better than calcium carbonate, whether taken on an empty stomach or with food.
In a randomized crossover study, patients were assigned to an 8-week calcium supplementation period and an 8-week control period. The subjects were given 1 g/day of calcium during the intervention period.
Sixty untreated or treated hypertensive patients (35 men and 25 women, mean age 58 years) with office systolic/diastolic blood pressure >= 140/90 mmHg.
The serum calcium concentration and urinary calcium excretion increased significantly with calcium supplementation. Office, home and 24 h blood pressure were lower in the calcium period than in the control period, although the differences were small (mean +/- SEM office blood pressure: 1.2 +/- 1.2/1.1 +/- 0.7 mmHg; home blood pressure: 1.9 +/- 0.7/1.3 +/- 0.6 mmHg; 24 h blood pressure: 1.2 +/- 0.8/0.9 +/- 0.5 mmHg,), and significant only for home systolic and diastolic blood pressures. (11)
A randomized, double-blinded, placebo-controlled trial was performed with 36 282 postmenopausal women, aged 50 to 79 years, who were already enrolled in the dietary modification and/or hormone therapy arms of the Women's Health Initiative clinical trial. Women were randomized at their first or second annual visit to receive a dose of 1000 mg of elemental calcium plus 400 IU of cholecalciferol (vitamin D) or placebo daily. Change in body weight was ascertained annually for an average of 7 years.
Calcium plus cholecalciferol supplementation has a small effect on the prevention of weight gain, which was observed primarily in women who reported inadequate calcium intakes. (16)
Numerous observational studies have found supplemental calcium and vitamin D to be associated with reduced risk of common cancers.
The purpose of this analysis was to determine the efficacy of calcium alone and calcium plus vitamin D in reducing incident cancer risk of all types.
This was a 4-y, population-based, double-blind, randomized placebo-controlled trial. The primary outcome was fracture incidence, and the principal secondary outcome was cancer incidence. The subjects were 1179 community-dwelling women randomly selected from the population of healthy postmenopausal women aged >55 y in a 9-county rural area of Nebraska. Subjects were randomly assigned to receive 1400–1500 mg supplemental calcium/d alone (Ca-only), supplemental calcium plus 1100 IU vitamin D3/d (Ca + D), or placebo.
When analyzed by intention to treat, cancer incidence was lower in the Ca + D women than in the placebo control subjects (P < 0.03). With the use of logistic regression, the unadjusted relative risks (RR) of incident cancer in the Ca + D and Ca-only groups were 0.402 (P = 0.01) and 0.532 (P = 0.06), respectively. When analysis was confined to cancers diagnosed after the first 12 mo, RR for the Ca + D group fell to 0.232 (CI: 0.09, 0.60; P < 0.005) but did not change significantly for the Ca-only group.
Improving calcium and vitamin D nutritional status substantially reduces all-cancer risk in postmenopausal women. (27)
In 1999 Howard J. Heller, MD and his colleagues compared the calcium absorption of calcium citrate and calcium carbonate supplementations after a single oral dose (500 mg calcium), taken with a meal.
This study was conducted to compare pharmacokinetic indices of calcium absorption after a single oral (500 mg calcium) load of calcium citrate and calcium carbonate.
In conclusion, calcium citrate was shown to be much more bioavailable than calcium carbonate. (28)
1. Chevalley T., Rizzoli R., Nydegger V., et al. Effects of calcium supplements on femoral bone mineral density and vertebral fracture rate in vitamin D-repleted elderly patients. Osteoporosis Int. 1994;4:245-52.
2. Dawson-Hughes B. Calcium, vitamin D and vitamin D metabolites. Osteoporosis 1996. Ed. S.E. Papapoulos et al. Elsevier. Amsterdam, Lausanne, New York. 1996; 299-303.
3. Bostick RM, Kushi LH, Wu Y, et al. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am J Epidemiol 1999; 149:151-61.
4. Bell L, Halstenson CE, Halstenson CJ, et al. Cholesterol-lowering effects of calcium carbonate in patients with mild to moderate hypercholesterolemia. Arch Intern Med 1992;152:2441-4.
5. Shils ME. Modern Nutrition in Health and Disease. 9th ed. Baltimore: Williams & Wilkins, 1999.
6. Riggs BL, Melton L. The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone 1995;17:505S-511S.
7. National Osteoporosis Foundation. NOF osteoporosis prevention - risk factors for osteoporosis. 2003.
8. Rouse IL, Beilin LJ, Armstrong BK, Vandongen R. Blood-pressure-lowering effect of a vegetarian diet: controlled trial in normotensive subjects. Lancet 1983;1:5-10.
9. Margetts BM, Beilin L, Armstrong BK, Vandongen R. Vegetarian diet in the treatment of mild hypertension: a randomized controlled trial. J Hypertens 1985:S429-31.
10. Beilin LJ, Armstrong BK, Margetts BM, Rouse IL, Vandongen R. Vegetarian diet and blood pressure. Nephron 1987;47:37-41.
11. Allender PS, Cutler JA, Follmann D, Cappuccio FP, Pryer J, Elliott P. Dietary calcium and blood pressure. Ann Intern Med 1996;124:825-831.
12. Bucher HC, Cook RJ, Guyatt GH, et al. Effects of dietary calcium supplementation on blood pressure. JAMA 1996;275:1016-1022.
13. Davies KM, Heaney RP, Recker RR, Lappe JM, Barger-Lux MJ, Rafferty K, Hinders S. Calcium intake and body weight. J. Clin Endocrinol Metab 2000;85:4635-8.
14. Heaney RP. Normalizing calcium intake: projected population effects for body weight. J Nutr 2003;133:268S-70S.
15. Zemel MB. Regulation of adiposity and obesity risk by dietary calcium: mechanisms and implications. J Am Coll Nutr 2002;21:146S-51S.
16. Calcium Plus Vitamin D Supplementation and the Risk of Postmenopausal Weight Gain Arch Intern Med. 2007;167:893-902
17. Holick MF. Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004;79(3):362-371. (PubMed)
18. Griffin MD, Xing N, Kumar R. Vitamin D and its analogs as regulators of immune activation and antigen presentation. Annu Rev Nutr. 2003;23:117-145. (PubMed)
19. Zeitz U, Weber K, Soegiarto DW, Wolf E, Balling R, Erben RG. Impaired insulin secretory capacity in mice lacking a functional vitamin D receptor. FASEB J. 2003;17(3):509-511. (PubMed)
20. Borissova AM, Tankova T, Kirilov G, Dakovska L, Kovacheva R. The effect of vitamin D3 on insulin secretion and peripheral insulin sensitivity in type 2 diabetic patients. Int J Clin Pract. 2003;57(4):258-261. (PubMed)
21. Heaney RP. Long-latency deficiency disease: insights from calcium and vitamin D. Am J Clin Nutr 2003;78:912-9
22. Parfitt AM. Osteomalacia and related disorders. In: Avioli LV, Krane SM, etc. Metabolic bone disease and clinically related disorders. 2nd ed. Philadelphia: WB Saunders. 1990:329-96
23. LeBoff MS, Kohlmeier L, Hurwitz S, Franklin J, Wright J, Glowacki J. Occult vitamin D deficiency in postmenopausal US women with acute hip fracture. J Am Med Assoc 1999;251:1505-11
24. Posner G. Low-Calcemic Vitamin D Analogs (Deltanoids) for Human Cancer Prevention. J. Nutr 2002;132:3802S-3S.
25. Martinez ME and Willett W C. Calcium, vitamin D, and colorectal cancer: a review of the epidemiologic evidence. Cancer Epidemiol. Biomark. Prev 1998;7:163-68.
26. Sakhaee K, Poindexter JR, Griffith CS, Pak CY. Stone forming risk of calcium citrate supplementation in healthy postmenopausal women. J Urol. 2004 Sep;172(3):958-61.
27. Joan M Lappe, Dianne Travers-Gustafson, K Michael Davies, Robert R Recker and Robert P Heaney Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial
28. Heller HJ, Stewart A, Haynes S, et al. Pharmacokinetics of calcium absorption from two commercial calcium supplements. J Clin Pharmacol. 1999;39:1151–1154.
29. Tuck SP, Datta HK. Osteoporosis in the aging male: treatment options. Clin Interv Aging. 2007;2(4):521-36.
30. Gennari C. Calcium and vitamin D nutrition and bone disease of the elderly. Public Health Nutr. 2001 Apr;4(2B):547-59.
31. Masi L, Bilezikian JP. Osteoporosis: new hope for the future. Int J Fertil Womens Med. 1997 Jul-Aug;42(4):245-54.